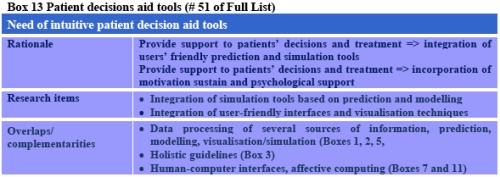
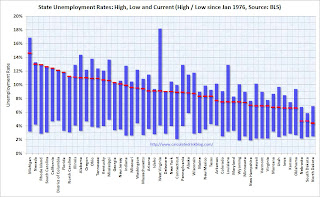
New Physician Adoption StatisticsTuesday, January 26th, 2010 | Posted by: Dr. David Blumenthal | Category: ONCThe CDC recently released its latest report on the adoption of electronic health records/electronic medical records (EHR/EMR) amongst office-based physicians from the National Ambulatory Medical Care Survey. As a physician who trained and initially practiced in a time where nearly every order, record, and prescription was paper-based, the results are striking to me.
The final results for 2008 show about 16.7 percent of physicians reported having systems that met the criteria of a basic EHR/EMR system, and about 4.4 percent reported that of a fully functional system. Preliminary results for 2009 show about 20.5 percent reported having systems that met the criteria of a basic system, and 6.3 percent reported that of a fully functional system.
Combined basic and fully functional statistics for the last 3 years are as follows:
- 2007 – 17%,
- 2008 – 21%,
- Preliminary 2009 – 27%
The latest figures, especially the preliminary 2009 numbers, suggest that the pace of adoption of HIT is quickening. We expect that the federal government’s health IT strategy will accelerate the pace even further by systematically addressing the obstacles physicians experience in adopting health IT (see below).
HOW THE US FEDERAL GOVERNMENT IS SUPPORTING HEALTH INFORMATION TECHNOLOGY USE
The Obama administration believes health information technology (HIT) is a critical component of efforts to improve the quality, efficiency, and value of care delivered to patients. The Office of the National Coordinator for Health Information Technology (ONC) is leading the administration’s efforts to support the thoughtful application of HIT. Cognizant of the numerous barriers that exist to making health IT work in real-world settings, the ONC is administering programs to systematically address these barriers:
OBSTACLE INTERVENTION FUNDS Financial Resources Medicare and Medicaid Incentive Program: incentive payments to “meaningful users” who use health information technology to improve value and efficiency of care delivered to patients Technical Assistance Regional Extension Centers: Up to 70 regional extension centers (REC) will help providers through the process of selecting and implementing electronic health records $643 Million The vision of a health care system that uses information technology to improve the value of services to patients is inching closer towards reality.
The ONC is committed to making the transition to electronic health records successful for every physician and hospital.
I hope you will share the experiences, challenges, and success stories that belie these encouraging statistics.
– David Blumenthal, M.D., M.P.P. – National Coordinator for Health Information Technology
National Coordinator for Health Information Technology, David Blumenthal, MD, blogs about physician adoption of electronic health records, a subject on which he has long been the go-to authority. With merely 27% of physicians deploying a fully functional EHR, its now up to Blumenthal to find real solutions and strategies for stimulating widespread adoption. So far his ideas and initiatives have been promising.

![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_a.png?x-id=0d8ff51d-41da-4bf1-8862-cca461979358)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_a.png?x-id=c96d68c2-cadf-419f-86d7-a13974f663f8)

